Anatomy is one of the oldest sciences that describes the human form. These descriptions are based on observations of as well as insights in the human form of those days. Over the centuries many anatomical books were written. Often as a copy of previous editions. Over the centuries a certain way of looking was passed from one generation to the next. By copying books we also copied our way of looking at form and function. Question: can a change of looking turn into the capability of seeing different forms and functions which are now still hidden behind the old Nomina Anatomica?
Anatomical rethoric
According to the anatomical literature we distinguish 7 cervical, 12 thoracal and 5 lumbar vertebra. The vertebral column is last but not least completed by a sacral and coccygeal bone. This caudal region, together with both iliacal bones is referred to as the Pelvis.
Looking more closely to that region, we can notice that the sacral and coccygeal bone are ossifications of respectively 5 sacral and 4 coccygeal vertebra (some authors speak of 3 coccygeal). Although it looks on the outside as one bone, in a sagittal cut it becomes clear that the sacrum remains 5 individual vertebra because the ossification mainly appears in the cortical part of the bone. This is more difficult to observe for the coccygeal bone, nevertheless, its origin is also still observable. So, why not speak of a vertebral column consisting of 7 cervical, 12 thoracal and 5 lumbar vertebra which is completed by 9 pelvic vertebra?
Although rare, it does happen that the 5th lumbar vertebra ossifies with the sacral bone. This phenomenon is known as the sacralisation of L5. In most cases it appears only on one side of the vertebral column. Looking more closely to this phenomenon of sacralisation it becomes obvious that it is not such a strange idea to define the presence of 6 sacral vertebra (L5 + 5 sacral). Consequently, we could alter our nomenclature by redefining that 5th lumbar into the 1st sacral vertebra. And this leads to the possibility of defining 10 pelvic vertebra: 6 sacral + 4 coccygeal. This mind game may cause a smile or even disbelieve that raises the question: why should we do this? Isn’t this just a silly mental exercise? And to what end? Let us have a look.
The mechanism behind ossification
Connective tissue is also known as inner tissue or mesoderm (the latter both embryological term). This connective tissue comes in a broad variety. It appears in a liquid state (blood) as well as a solid state (bone). And in between we have any kind of appearance such as fascia, tendon, ligament, etc..
When connective tissue leans more towards a liquid state, its form and function are favouring chemical (metabolic) exchange due to the high permeability – support against physical strain however is low. Looking to the other extreme, connective tissue that leans towards a solid state such as bone, its form and function favours mechanical support against physical strain – support for a chemical exchange is low.
Studying the phenomenon of life, we can observe that it is characterized by a constant change of form (adaptation). This change is according to environmental conditions. We can conclude that life in fact is a constant search of an optimized state. A State that allows sufficient chemical (metabolic) exchange while a certain physical resistance against for instance gravity is guaranteed – and vice versa.
Ossification of connective tissue is a journey of constant change starting in a liquid state towards a solid state. It is a question of the proportional presence of the four components of connective tissue: water, matrix, cells, fiber – chronologically present in this order. The German embryologist E. Blechschmidt calls the region in which ossification takes place a densation field. These densation fields can be observed throughout many developmental stages but also till long after birth. In fact, densation fields occur throughout our entire life. In certain circumstances these changes of texture are even defined as pathologies such as osteophytosis or calcification of the supraspinatus tendon in the shoulder region. Or what to think of the plantar spur? All of them are examples of (re)active densation fields.
One of the common characteristics of these changes in density is the fact that these fields are areas where water gets pushed out of the region while the matrix is captured between the fibers. The connective tissue becomes more dense. Consequently, its metabolic exchange reduces while the supporting feature for physical strain increases. Although chemical processes cannot be excluded in the ossification process, the importance of the physical features in the process of transformation cannot be denied. On the contrary!
Physical conditions leading to densification
DEVELOPMENTAL CONDITIONS
Inflation growth – Development of the vertebral column is characterized by a number of chronological steps. To begin with there is the compressive influence of frontier tissue growth such as that of the future neural tube. This compressive influence has an immediate impact on the neighbouring cells of the inner tissue. The region where these future connective tissue cells become compressed is defined as a contusion field. Within this field young cartilage cells are developed. These cells, beside their altered form, also show a different metabolic behaviour that becomes evident in the appearance of fibers in their direct surrounding.
Development does not only happen in a certain chronology but also in phases. We clearly can distinguish phases of metabolic activity alternated by moments of relative metabolic rest. The active metabolic phase of the neural tube causes the compression of neighbouring inner tissue cells. After this active phase we can observe a moment of relative rest during which the phenomenon of expansion growth can be observed. This expansion growth comes from the young cartilage cells that were developed within the contusion field. When the compression starts to diminish, the inner tissue cells begin to suck in water. This phenomenon is a consequence of the oncotic pressure. Oncotic pressure, also called colloid osmotic pressure, is exerted by proteins which tend to attract water. Since water was pushed out of the cells, the concentration of proteins within the cell increases and consequently their oncotic influence. As soon as this oncotic pressure increases, it is as if these cells begin to inflate like a balloon due to the increasing volume of water content. This is a specific characteristic of a distusion field in which adult cartilage is developed.
This inflation growth, where inner tissue cells push each other aside, will put the fibers of the inner tissue under physical strain (retension field). Consequently, the water between the cells and fibers is pushed out of that region leading to densification. This phenomenon turns the cartilage into enchondral bone.
Developmental movement – But not only inflation growth of cartilage leads to an increase of physical stress on the young connective tissue. Developmental movements of organs as organ systems as well can and will cause an increase of a physical strain within the fibers of that connective tissue. Hence also on the future vertebral column. Since the development can be described as a movement, one of the characteristics of that movement becomes apparent within the features of the fibers: the fibers receive a spatial orientation. Fibers in a retension field show a clear direction. In structures such as ligaments and tendons this becomes quite evident. A densified form of these fibers is also present in bony structures. In that case we talk of trabeculae. They too have a distinct spatial orientation! It is an orientation in continuity with the fiber direction of neighbouring and less dense connective tissue. Traces of developmental movements related to organs are eminently present within the structuration of bones!
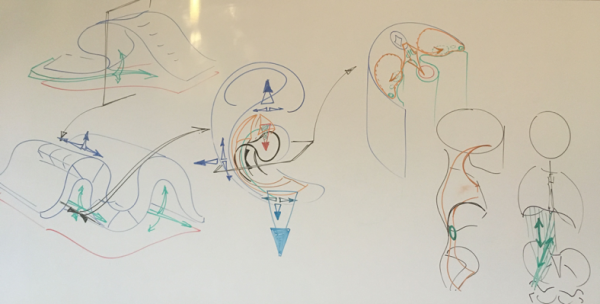
Illustration 1 (left): Schematic presentation of the pelvic region.
The green color represents the mesothelial frontier tissue which will become the future peritoneum – in this case specifically the peritoneum parietal pelvis. In the posterior wall the imprints of the hindgut (red) as well as the gonads (black) can be distinguished. The green folds on either side will become the Fallopian tubes (Ductus of Müller, also called paramesonephric duct – only in female). In alignment to these structures we can distinguish developmental pattern that will cause strain within the inner tissue space (future pelvic and retroperitoneal space).
Developmental relationships are indicated by the orange arrows. The posterior arrows indicate developmental relationship with retroperitoneal space (for instance Lig. Suspensorium ovarii). Anterior arrow indicates relationship with Lig.teres hepatis and continuity towards diaphragm.
Illustration 2 (right): Schematic presentation of the pelvic region.
Developmental relationship with Cran.Vert.Sacr.Syst. and abdominal diaphragm as well. The schematic representation indicates the numerous possibilities regarding positional relationships between different system. Noticing the directional features within these positional relationships is seeing the possible impact of the functionality in specific regions.
Source: Anatomy & Ontogenesis – Seminar 4: Developmental pattern of the urogenital system; La Bresse/France, 2019
GRAVITATIONAL CONDITIONS
Once we are born, one of the most confronting changes is gravity. It puts a strain on our body. This strain has an enormous impact on our connective tissue. In the attempt of dealing with this physical stress, forces are guided into the direction of less resistance. With other words, the fibers of our loose connective tissue become even more organised. And what about those who are already spatially, directionally organised? These fibers become reinforced by an increasing number as well as by a push-out of fluid.
A distinct feature of the increasing number of fibers as well as their densification is that their direction of less resistance (of ease) corresponds to the direction of the developmental pattern which were “already pre-installed” by the developmental movement of organs and organ systems! This leads us to the conclusion that our behaviour under gravitational circumstances enforces the existing characteristics of structuration and texture (density) resulting from prior developmental movements.
ABOUT THE PELVIC VERTEBRA
In relationship to the pelvic region we have to distinguish a difference between the larger and the minor pelvis. The larger, the broader part of the pelvis mainly refers to both iliac parts. The minor pelvis refers to the region that includes the sacral and coccygeal bone as well as the Os ischium (and partially pubic bone).
The form and function of the minor pelvis is intimately related to the development of the urogenital organs. In fact, their developmental movements cause a directional strain within the connective tissue of the pelvic region. This directional strain, these developmental patterns, change the state of the connective tissue by densifying its texture. This transformation of the pelvic region is an on-going event that takes place till long after birth! This post-partum change of the pelvic form becomes for instance evident during the puberty of young females prior to and during the first menstruations. Not forgetting to mention the period of pregnancy where the pelvic form changes as well! (for the biochemists among us: yes, metabolic changes do have an influence on the texture of the connective tissue, “preparing” the coming birth – although this “preparing change” should be more considered as a consequence of that changing chemical AND physical condition within that region).
Supplementary influence of gravity, especially increasing due to the changing posture (bipodal position), enforces the strain on the connective tissue and speeds up the densification process. It enforces the strain on the already present directional features of the fibers. And this leads to a transformation of the pelvic region.
Lumbar 5 should be called sacral 1
When we study thoroughly the movements of the structures involved in the urogenital development, it becomes obvious that the directional strain of this event extends far into the so-called lumbar region. Structures such as the Lig. Suspensorium ovarii extend fan-shaped into the region of vertebra lumbar 5. Within that same region there are other changes of textures as well. Ligaments such as the iliolumbar are clearly densifications that appear from strain partially caused by the developmental movements of the urogenital organs. In later life, these structures are put under additional strain by gravity as soon as the individual comes into an upright (bipodal) position.
In anatomy as well as embryology books this so-called Lig. Suspensorium ovarii is only described in female. However, we should keep in mind that the descending movement of the ovaries can be described for the testis as well. The gonads of both genders undergo (almost) the same developmental conditions. There may be some gender specific differences, the tendency of the developmental movement is however the same.
This movement causes a strain and consequently a densification of the inner tissue (future connective tissue). This change in texture leads in both genders to the same traces of fiber organisation. Depending on the extend of identification, it becomes known under a specific anatomical nomenclature for a specific structure, … or not. As an example: the male Gubernaculum equals the female Lig. Teres uteri where the female Lig. Suspensorium ovarii equals in male … apparently to nothing. Is it? Looking into the microscopic dimensions of the connective tissue of that region, the constitution of the connective tissue in that region will tell differently! (A.T. Still, Philosophy of Osteopathy, Page 17-18: what I mean by anatomy)
(For the anatomy lovers among us, here is a teaser: what about the ligament of Clado between the broad ligament and appendix? Is this an anatomical reality or just the imagination of an French gynaecologist 1856-1905; Stedman’s Medical Eponyms)
Form is a consequence of its structures and their positional relationships. Function is a constant attempt to maintain that original form. Function is a constant resistance against a change in the positional relationship. In that context the 5th lumbar vertebra is a structural part of the spinal column. But due to its positional relationships most definitely also a structural component of the urogenital system in the pelvic region. Consequently, it makes sense to call this L5 the 1st pelvic vertebra! Due to the intimate relationship with the urogenital apparatus it makes more sense to use exactly this nomenclature. A relationship that gives the pelvic region its specific form and function!
Anatomical reality or just a brain game?
The brain game of redefining anatomical structures, how realistic is it? And to what end? The question we can ask ourselves is: besides the rare phenomenon of the sacralisation of L5, are there other anatomical and/or functional indications for the assumption that this vertebra should be seen as the 1st sacral one (or the 1st of 10 pelvic vertebra)?
TISSUE ORIGIN OF LOW BACK PAIN
In 1991, Kuslich and his colleagues published an article under the title “The tissue origin of low back pain and sciatica” (Orthopedic Clinics of North America, Vol.22 No2). The most interesting conclusion of their investigations is that lumbar pain as well as sciatica could only be explained by the presence of an inflammation of the nerve root. Pulling and pushing on the skin, muscles, ligaments, articular capsules, discs, … none of these tissues could be linked to the sensation of the patient with lumbar pain and/or sciatica!
Looking deeper into the physiological origin of tissue inflammation several conclusions can be made. To begin with: only connective tissue can become inflamed! And inflammation clearly has a vascular background. The latter means that all too often, if not always, congestion within the vascular system is a significant clinical sign of inflammation. This congestion is related to the form and function of the veno-lymphatic part of our vascularisation. And now it becomes interesting.
VASCULARISATION OF L5
Low back pain, as well as sciatica, is a frequent reason for patients to visit an osteopath. A detailed knowledge of the vascularisation of that region should therefore be a primary condition in order to be able to understand what is causing that symptom.
Can it be a vertebra that is locked into a certain position (FRS, ERS, NSR – see laws of Fryette)? Yes, why not. But this does not answer the question who or what has changed the positional relationship of that vertebra in regard to its neighbouring structures. The common explanation/pseudo-excuse of “having lifted something wrong” of “did a wrong movement” is too simplistic and by far not the only reason; what about those patients who “woke up with it”? Neither does the concept of the “dysfunction” of a vertebra realy explain the explicit features of “chemical pain” (diffuse, increase in case of immobility, referred to as C-fiber pain, etc.). A chemical pain that is so specific in the case of inflammation. Inflammation, which is, according to the findings of Kuslich et al, a very important clinical condition for lumbar and sciatic pain.
In the case of inflammation, the attention should be brought to the (micro)vascularisation of the region where the symptom is occurring. So, what is the vascular contribution to that symptom and where does it come from? The first thing that is interesting to notice, anatomically, is the fact that the region of vertebra L5 is vascularized by a venous structure that does not connect directly to the Vena cava inferior but … how else can it be: the venous blood vessels of the pelvis. And in this specific case, although there are many variations, also the possibility to the venous blood vessels of the minor pelvis (urogenital!).
Additionally, we should not forget that these venous vessels do NOT have valves. This absence of valves leads to a non-fixed direction of the blood flow. Under normal conditions, we would expect that the 5th lumbar region drains into the pelvic region and from there to the internal iliacal vein, etc etc.. However, what in the case of pelvic (urogenital / rectal) congestion? Is it possible that the direction of the blood flow turns around? Well at least the pressure in these vessels goes up and this can cause congestion from the pelvis into that region of L5. Herlihy, in his publication of 1947 (revision of the venous system) even talks of a bypass from the pelvis into the vertebral column and from there directly into intracranial (dural) sinuses! So, according to Herlihy it is possible that blood can be shifted directly into the vertebral column. Batson (1956) describes these blood vessels of the vertebral column as venous store houses. His experiments show that the pelvic region is most definitely a preferred region for a shift of blood into the spine (see also Gilbert Breschet 1826). Unnecessary to mention is that when blood gets shifted into the veins of the vertebral column, that the pressure within the dural sinuses will rise as well. In the case that the venous shunts, such as the connection between the Sinus cavernosus and the Plexus pterygoideus is hindered, this increase of pressure can cause symptoms such as retro-ocular headache. The symptom may be in the cranial region and the pain may be in the lumbar. The initial cause for that problem however may be located in the pelvic region.
So, looking more detailed into the vascularisation of the vertebra L5, we notice this intimate relationship with blood vessels of the pelvic region. Consequently, it should not surprise that pattern of strain within the structures related to the urogenital system, located in the pelvis, include and extend to all other structures which are positionally and directionally related to each other. Consequently, it should not surprise that a treatment of the surrounding “suspension” apparatus of the urogenital system has an impact on the congestion phenomenon of the pelvic region, including L5 (and even in the cranial region)! A treatment of the fascias, ligaments and other densified areas of the connective tissue (including bony trabeculae) in relationship to that region will have an impact on the vascularisation of L5 (or should we say vertebra pelvis 1?). This treatment can be seen as a treatment of the cranio-vertebro-sacral system as well as the visceral system. It is just a matter of defining “the characteristics of the system” in relationship to the region of the symptom – to which system does the connective tissue strain in form of a pattern belong?
Illustration 4: Schematic presentation of the different developmental stages leading to the structuration of the retroperitoneal space.
The so-called retroperitoneal space is in fact a continuity of the thoracal located mediastinum that extends into the pelvic region. This “inner tissue space” contains the major neuro-vascular components for each individual system: Cran.Vert.Sacr., Visceral, urogenital and Loco.Mot. Syst.. Moreover, this space unites these different systems – in many ways (functional and dysfunctional).
Please keep in mind that each color as well as each arrow in this scheme represent a so-called restraining apparatus. An apparatus that represents an anatomical structure and a positional relationship. Each color and each arrow can be representating a blood vessel, a nerv, a muscle, a fascia, a tendon,… . Although these structures have different textures (different densities), they do have one thing in common: trajectorial features. These trajectories are structured developmental pattern which become preferred directions of ease when the human body is responding to its environmental stress.
Source: Anatomy & Ontogenesis – Seminar 4: Developmental pattern of the urogenital system; La Bresse/France, 2019
ABOUT MUSCULUS PSOAS MAJOR AND MORE
The special vascularisation of the vertebra lumbar 5 is not the only anatomical indication for the fact that this vertebra should receive another name. Looking at the Musculus psoas major it is clear that this muscle “inserts” up until vertebra L4. Why not up until L5? Moreover, why is the Truncus lumbosacralis located at L4-L5 and not L5-S1? It only makes sense when we see the 5th lumbar vertebra as a part of the pelvic region. A region that extends into a certain compartment of the limbs that continuous along a neurovascular axis related to the sciatic nerve … . What was the tissue origin of the sciatic pain again? Exactly!
What do you do in the case of?
What do you do in the case of for instance a lumbar pain, or a sciatic pain, or …? Which technique do you use, a high velocity trust or rather a Sutherland technique? Or, how valuable is a muscle energy technique in the light of Kuslich’s discovery (muscles are no origin for)?
To begin with, “what do you do in the case of” begins with an anatomical understanding of the patient’s problem. And this is more than just knowing some anatomical structures by name and by heart! It is about form, structures and positional relationships. Knowing what it means is knowing about “the normal” (see A.T. Still). And this goes beyond the borders of the macroscopic dimensions. Positional relationships become obvious (logical) as soon as they receive a spatial organised directional context. A context described in form of a pattern, a knowledge that becomes obvious for example during embryological studies.
And then there is the question of what technique. The modus operandi “this symptom = that technique” is a very strong simplification (A.T. Still, Philosophy of osteopathy, page 2: I do not instruct the student to punch or pull a certain bone, … for a certain disease, …). A simplistic approach which is only required by those who do not know their anatomy. Or using the words of A.T. Still: they have nothing to reason from (Autobiography, chapter 12, page 162). Therefore, they do not understand the patient’s problem!
Techniques are merely tools. Looking into the nature of tissue response to physical as well as chemical conditions, we can observe that two “physical forces” play a significant role: compression and traction forces. So why not use this with more awareness? In fact, we should ask ourselves not so much which technique we should use but much more the question what direction we should go to in order to release the strain within the connective tissue. Isn’t this a very simple but nevertheless important principle?
But what does it mean without the importance of visualising this strain in the picture of a living anatomical form? Isn’t this an essential condition for the application of any kind of so-called technique? The least we can say is that it is an essential contribution to the accuracy of our technical intervention (A.T. Still, Autobiography, The philosophy and mechanical principles of Osteopathy, page 18: … one thousand of an inch …). A picture that not only contains all present structures but also their positional relationships to other structures. Isn’t this a condition in order to be able to distinguish what is normal and abnormal?
Conclusion
Redefining the anatomical nomenclature based on the accurate description of positional relationships between anatomical structures gives us a more accurate image of our patient and his/her problem(s). Problems which are not his/her symptoms but the changes within these relationships . Changes that cause different ways of behaving!
In order to discover historically hidden relationships due to classic nomenclature, it takes a different way of looking at the anatomical form. An understanding of the principles behind the development of this form can help us to change that way of looking in order to see new positional relationships. It can help us to give another meaning to the term “(dys)function”.
In a technocratic society, where apparently techniques come before anything else, the new credo should be: Do not ask me how I have done it, ask me why I have done it (*). A profound knowledge of anatomy, based on insights from the past as well as of the presence, is a condition to be able to answer the latter.
______________________________
(*) These words do not come from Andrew Taylor Still but I am pretty sure he would agree.